Guided bone regeneration: here's how to restore lost bone
Did your dentist tell you that you don't have enough bone to insert the implant? Did they talk to you about bone grafting and you don't know what it is? Here is what guided bone regeneration is all about.
 Returning to smile is the dream of many. Each patient has various prosthetic solutions available for his mouth but undoubtedly desires the best.
Returning to smile is the dream of many. Each patient has various prosthetic solutions available for his mouth but undoubtedly desires the best.
How often do you hear yourself say "you have little bone", cutting, in fact, all the possibilities to insert a dental implant?
Actually, nowadays, thanks to the new surgical techniques it is possible to resort to bone regenerative, recovering all the lost bone in a few months.
Let's find out what it is all about.
When the volume of the alveolar bone becomes particularly small, its dimensions are no longer sufficient to house the implant screws, making a regenerative operation necessary.
Among the most used methods stand out the use of growth factors, split crest, and guided bone regeneration (called GBR), where the latter procedure has greater scientific evidence.
In particular, after the loss of the teeth, the bone that previously enveloped the root undergoes marked reabsorption in the first 6 months and then continues over time in a slow but still constant manner.
Resorption of the maxillary bone and mandible represents a challenge for the implantologist, as it will be his task to determine whether and how to insert the implants in the affected area.
Class 1: alveolar ridge with the tooth in place;
Class 2: post-extraction socket, or bone volume present after tooth extraction;
Class 3: rounded ridge but of sufficient height and thickness;
Class 4: knife blade crest. Suitable height but inadequate thickness;
Class 5: flat ridge with unsuitable height and thickness;
Class 6: depressed or absent alveolar bone (only in the mandible).
This subdivision is extremely important and its evaluation is done radiographically by 3D CT. In classes I, II, and III it is possible to insert implants without resorting to surgical techniques of bone augmentation. On the other hand, a correction of the volume is necessary
bone.
 bone regeneration (GBR) involves the use of membranes in association or not with filler materials called graft materials.
bone regeneration (GBR) involves the use of membranes in association or not with filler materials called graft materials.
The objective of this treatment is to recreate a suitable bone volume in order to then be able to insert implants in an optimal position for the subsequent prosthetic rehabilitation.
In a nutshell, it is an intervention that consists of opening a flap at the level of the oral mucosa until it detects the underlying atrophic bone. Then we proceed with the insertion of a membrane and any filling material and it closes. Months later we will see bone regeneration.
Like suture threads, they can either undergo spontaneous degradation (resorbable membranes) or may require a second surgical procedure to remove them (non-resorbable membranes).
To perform their task, the membranes must have a series of requirements:
- Biocompatibility. In order not to trigger an immune response from the body;
must act as a semipermeable barrier. Allowing the exchange of nutrients but preventing the passage of cells;
- Stability; easy handling for the implantologist who must position it.
 non-resorbable membranes are undoubtedly the most used in guided bone regeneration. As the word itself says, after their positioning, they do not undergo a process of degradation but need a second intervention to be removed.
non-resorbable membranes are undoubtedly the most used in guided bone regeneration. As the word itself says, after their positioning, they do not undergo a process of degradation but need a second intervention to be removed.
They consist of expanded polytetrafluorethylene (e-PTFE) and in some variants, there is the presence of thin titanium sheets that amplify the maintenance of the space. Titanium sheet regenerative
 type of membrane is made of biodegradable materials that allow avoiding a second intervention for their removal. For example, collagen membranes usually undergo a spontaneous degradation process within 4-8 weeks.
type of membrane is made of biodegradable materials that allow avoiding a second intervention for their removal. For example, collagen membranes usually undergo a spontaneous degradation process within 4-8 weeks.
In guided bone regenerative, resorbable membranes are less used both for their more frequent tendency to collapse and for the difficulty in finding a material that can undergo re-absorption in suitable times.
Regarding the classification of filler materials, these are divided into:
- Autologous bone, taken from the same patient;
- Homologous bone, typically from a corpse;
- Heterologous bone, of animal origin;
- Synthetic bone.
Furthermore, as it is human bone, it is reshaped in the correct physiological times and is, therefore, the best usable bone substitute.
The main disadvantage of autologous bone is represented by the need to perform a withdrawal from intraoral sites of the patient himself, such as the body and the jaw branch.
Cases with extraoral withdrawals, typically from the hip, have also been described, but they are quite rare.
- Homologous bone
- Homologous bone can be taken from a living donor or from a corpse, in the latter case within 24 hours of death.
In living donors, the bone is derived from operations on the hip, femur, tibia, humerus, ribs, and vertebrae.
To prevent the inevitable unleashing of the immune reaction of the receiving organism, the homologous bone is treated. However, several studies show a low tendency to resorption.
However, they are still little known and used bone substitutes.
The most commonly used are biofuels, but further scientific studies are still needed.
This is because the grafted bone must first integrate with the surrounding tissue, and only later can it be "loaded" prosthetically.
 Returning to smile is the dream of many. Each patient has various prosthetic solutions available for his mouth but undoubtedly desires the best.
Returning to smile is the dream of many. Each patient has various prosthetic solutions available for his mouth but undoubtedly desires the best.How often do you hear yourself say "you have little bone", cutting, in fact, all the possibilities to insert a dental implant?
Actually, nowadays, thanks to the new surgical techniques it is possible to resort to bone regenerative, recovering all the lost bone in a few months.
Let's find out what it is all about.
What is regenerative bone surgery?
The term regenerative bone surgery indicates a set of surgical methods aimed at restoring the bone structure in terms of height and thickness so as to ensure the conditions for correct positioning of the dental implants.When the volume of the alveolar bone becomes particularly small, its dimensions are no longer sufficient to house the implant screws, making a regenerative operation necessary.
Among the most used methods stand out the use of growth factors, split crest, and guided bone regeneration (called GBR), where the latter procedure has greater scientific evidence.
Bone resorption
Normally, any bone in the body undergoes a remodeling activity consisting of apposition and resorption. In physiological conditions, there is a balance between the two phases, but when the resorption prevails there is bone atrophy.In particular, after the loss of the teeth, the bone that previously enveloped the root undergoes marked reabsorption in the first 6 months and then continues over time in a slow but still constant manner.
Resorption of the maxillary bone and mandible represents a challenge for the implantologist, as it will be his task to determine whether and how to insert the implants in the affected area.
Types of reabsorption
In 1988 Dr. Cawood and Dr. Howell performed classification on the various types of reabsorption dividing the degrees of atrophy into 6 classes:Class 1: alveolar ridge with the tooth in place;
Class 2: post-extraction socket, or bone volume present after tooth extraction;
Class 3: rounded ridge but of sufficient height and thickness;
Class 4: knife blade crest. Suitable height but inadequate thickness;
Class 5: flat ridge with unsuitable height and thickness;
Class 6: depressed or absent alveolar bone (only in the mandible).
This subdivision is extremely important and its evaluation is done radiographically by 3D CT. In classes I, II, and III it is possible to insert implants without resorting to surgical techniques of bone augmentation. On the other hand, a correction of the volume is necessary
bone.
Guided bone regeneration (GBR)
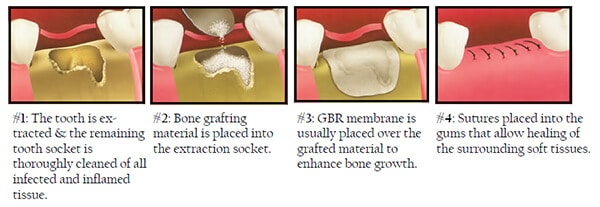
 bone regeneration (GBR) involves the use of membranes in association or not with filler materials called graft materials.
bone regeneration (GBR) involves the use of membranes in association or not with filler materials called graft materials.The objective of this treatment is to recreate a suitable bone volume in order to then be able to insert implants in an optimal position for the subsequent prosthetic rehabilitation.
In a nutshell, it is an intervention that consists of opening a flap at the level of the oral mucosa until it detects the underlying atrophic bone. Then we proceed with the insertion of a membrane and any filling material and it closes. Months later we will see bone regeneration.
The membranes
The membranes are thin semipermeable sheets that are applied between soft tissue and bone. Their use is essential to isolate the area to be regenerated and to favor the formation of the clot, necessary for correct guided bone regeneration.Like suture threads, they can either undergo spontaneous degradation (resorbable membranes) or may require a second surgical procedure to remove them (non-resorbable membranes).
To perform their task, the membranes must have a series of requirements:
- Biocompatibility. In order not to trigger an immune response from the body;
must act as a semipermeable barrier. Allowing the exchange of nutrients but preventing the passage of cells;
- Stability; easy handling for the implantologist who must position it.
Non-resorbable membranes
 non-resorbable membranes are undoubtedly the most used in guided bone regeneration. As the word itself says, after their positioning, they do not undergo a process of degradation but need a second intervention to be removed.
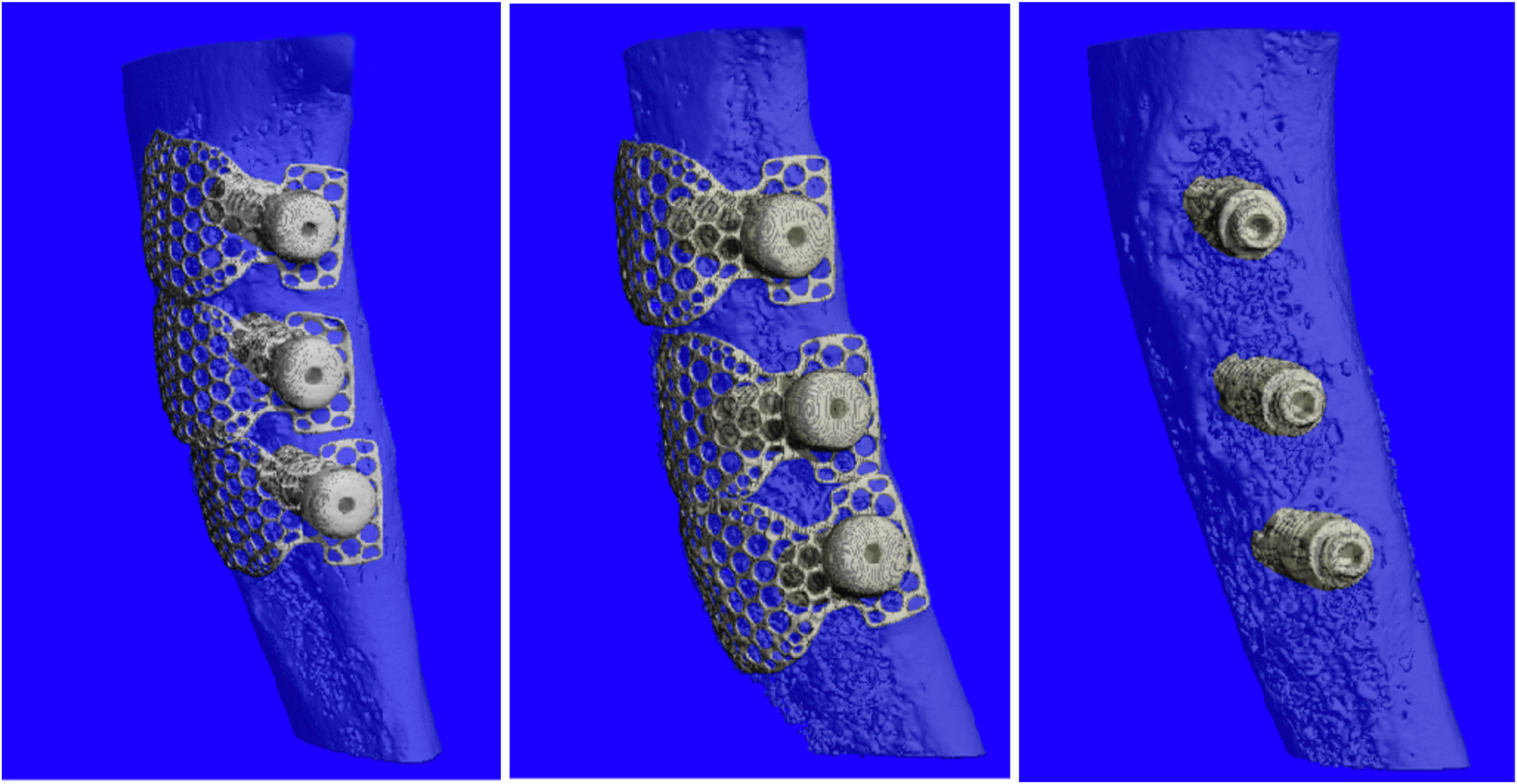
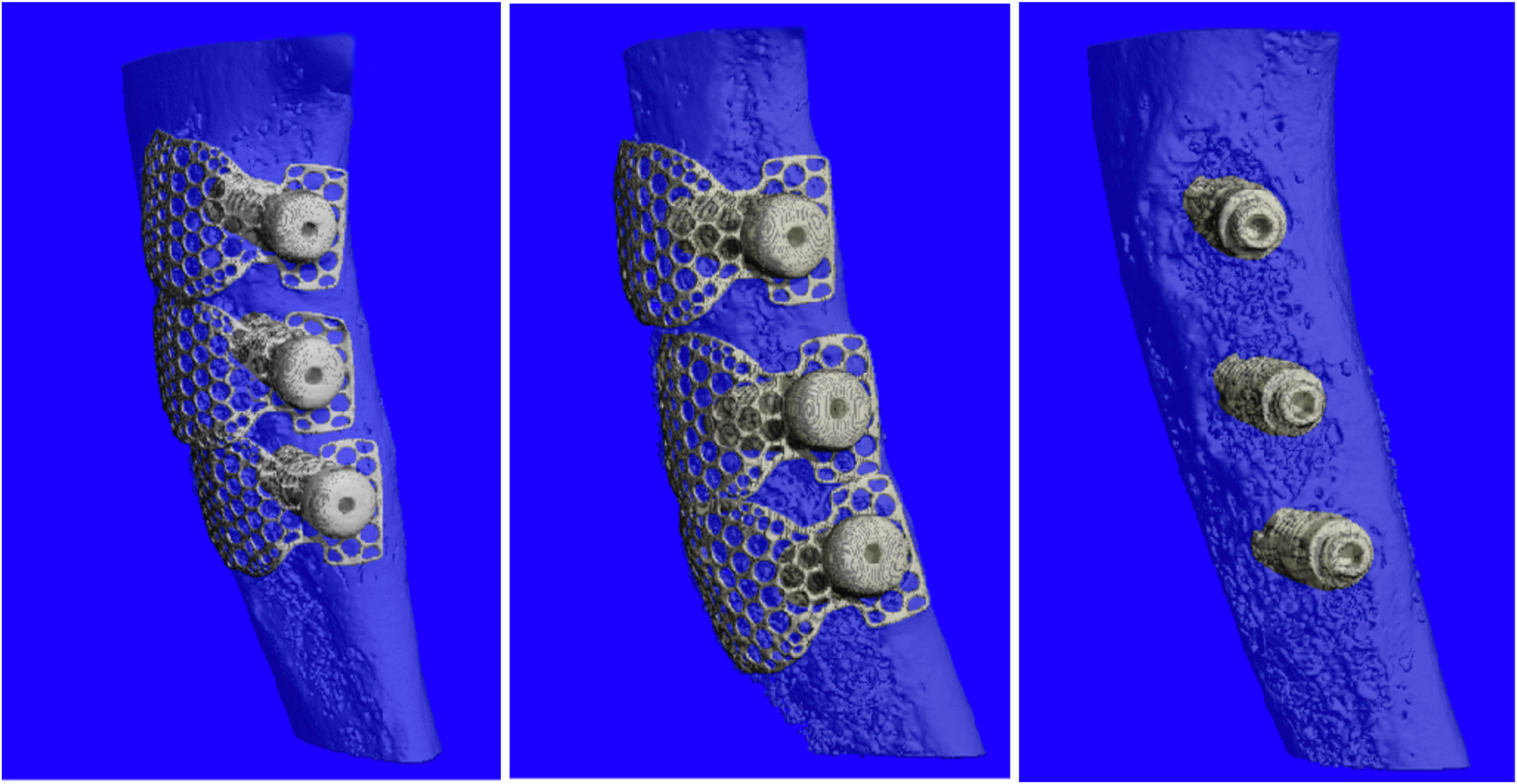
non-resorbable membranes are undoubtedly the most used in guided bone regeneration. As the word itself says, after their positioning, they do not undergo a process of degradation but need a second intervention to be removed.They consist of expanded polytetrafluorethylene (e-PTFE) and in some variants, there is the presence of thin titanium sheets that amplify the maintenance of the space. Titanium sheet regenerative
Resorbable membranes
 type of membrane is made of biodegradable materials that allow avoiding a second intervention for their removal. For example, collagen membranes usually undergo a spontaneous degradation process within 4-8 weeks.
type of membrane is made of biodegradable materials that allow avoiding a second intervention for their removal. For example, collagen membranes usually undergo a spontaneous degradation process within 4-8 weeks.In guided bone regenerative, resorbable membranes are less used both for their more frequent tendency to collapse and for the difficulty in finding a material that can undergo re-absorption in suitable times.
Regenerative membranes
Grafting materials
Filling materials, also called graft materials, are devices used to restore bone volume. These bone substitutes, in addition to having to be biocompatible as well, must behave as much as possible as the patient's own bone, therefore, be resorbable but also remodeling.Regarding the classification of filler materials, these are divided into:
- Autologous bone, taken from the same patient;
- Homologous bone, typically from a corpse;
- Heterologous bone, of animal origin;
- Synthetic bone.
Autologous bone
Coming from the patient himself, autologous bone guarantees the complete absence of immune reaction, resulting in perfectly tolerable.Furthermore, as it is human bone, it is reshaped in the correct physiological times and is, therefore, the best usable bone substitute.
The main disadvantage of autologous bone is represented by the need to perform a withdrawal from intraoral sites of the patient himself, such as the body and the jaw branch.
Cases with extraoral withdrawals, typically from the hip, have also been described, but they are quite rare.
- Homologous bone
- Homologous bone can be taken from a living donor or from a corpse, in the latter case within 24 hours of death.
In living donors, the bone is derived from operations on the hip, femur, tibia, humerus, ribs, and vertebrae.
To prevent the inevitable unleashing of the immune reaction of the receiving organism, the homologous bone is treated. However, several studies show a low tendency to resorption.
Heterologous bone
The heterologous bone substitutes currently most used are those of animal origin: bovine, equine, porcine. Among these materials, those of bovine origin make use of a long experimental and clinical experience and can be used alone or in association with autologous bone.Synthetic bone
In an attempt to create a material that encompasses all the ideal advantages, synthetic grafts have also been designed.However, they are still little known and used bone substitutes.
The most commonly used are biofuels, but further scientific studies are still needed.
Conclusions
Each type of graft material has advantages and disadvantages but in almost all cases of guided bone regeneration, there is a need to wait several months before inserting the artificial crown on the implant or even before inserting the screw into the bone.This is because the grafted bone must first integrate with the surrounding tissue, and only later can it be "loaded" prosthetically.
___________________________________________________________________________
Information brought you by Massimo - Write me with your Panoramic X-Rays view for a free specialist diagnosis just by sending an email to meditur@icloud.com
Information brought you by Massimo - Write me with your Panoramic X-Rays view for a free specialist diagnosis just by sending an email to meditur@icloud.com
DISCLAIMER
The Content above even if the above information is written or supervised by a professional in dentistry. A physical examination is a procedure by which the dentists investigate the oral cavity of patients for signs of disease. -- Together with the medical history, the physical examination aids in determining the correct diagnosis and devising the treatment plan. -- Always seek the advice of your physician or other qualified health providers with any questions you may have regarding your medical condition



Comments
Post a Comment